Crisis Assistance Response and Engagement (CARE) Dashboard
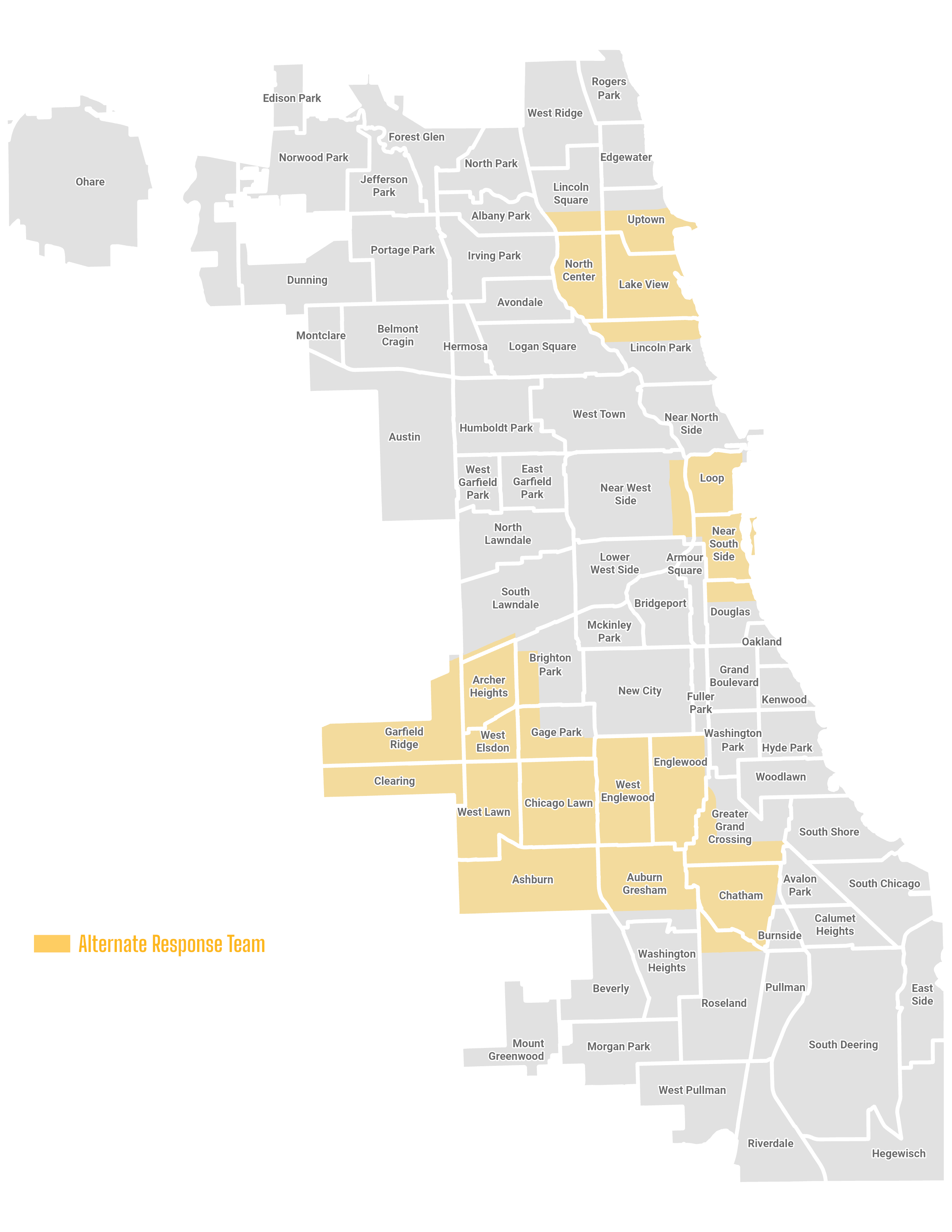
Chicago’s Crisis Assistance Response and Engagement (CARE) team seeks to ensure that individuals experiencing a mental health crisis and substance use overdose are assisted by teams of behavioral health professionals, with resources to address their unmet health and social needs. The CARE team responds to 911 calls with a mental health component Monday-Friday 10:30am-4:00pm in select community areas. When the CARE team responds to an individual in crisis they offer de-escalation, mental health assessment, referrals to community services, and transport to community-based destinations as appropriate. The CARE team conducts follow up at 1, 7, and 30 days with all individuals that they encounter.
The CARE Program is an initiative led by the Chicago Department of Public Health, with support from the Mayor’s Office and other city agencies. Crisis response teams comprised of CDPH behavioral health clinicians and CDPH emergency medical technicians ensure that residents experiencing a mental health challenge can receive compassionate and professional care, and connection to resources to address their unmet health and social needs.
For more information on the CARE Program, please contact: CAREProgram@cityofchicago.org
CARE in the Community
All names and genders in the stories here have been changed to
protect the privacy of individuals served by the CARE Team.

“Mark,” an individual experiencing homelessness, started a fire to try to keep warm. The fire got out of control, and the Chicago Fire Department was called. The CARE Team responded as an assist. Mark was very willing to speak with the CARE Team and stated that he wanted help. After assessing Mark, the CARE Team transported him to a community crisis stabilization center. The transport went well , and the CARE Team had great communication with the stabilization center, who was then able to get Mark into a shelter.

“Sharon” called 911 for a family member, “Aaron,” who was agitated, angry, and threatening to hurt themselves. Sharon reported that Aaron had shown signs of depression off and on, but that their behavior had worsened over the past days. Sharon reported that she called 911 as a last resort. She did not want Aaron to go to the hospital but also did not know what else to do. When the CARE Team arrived, they spoke with Aaron and each of the individuals in the household. The CARE Team noticed that everyone in the house was very anxious, and the decision was made to transport Aaron to a crisis clinic rather than a hospital in an ambulance. During the ride to the clinic, the CARE Team Clinician was able to learn more about Aaron and develop trust. When the CARE Team arrived at the clinic, Aaron was calm, engaged with the CARE Team and open to seeing a therapist.

The CARE Team responded to an individual in crisis, “Candice,” who needed to go to the hospital for a psychiatric evaluation. When speaking with Candice, the CARE Team Clinician discovered that her refrigerator was broken, and she needed assistance completing insurance forms. While Candice was in the hospital, the Clinician worked to set up hot meal delivery, connected with SNAP, and assisted with filling out insurance forms. The Clinician also worked to get Candice a new PACE card and access to consistent therapy and medication.

The CARE Team responded to assist police through a potential threatening suicide call. The Team discovered that the individual on the call, “Luis,” was not suicidal, but needed help addressing domestic violence in their residence and related mental health concerns. The Clinician on the team worked to connect Luis to outpatient mental health treatment that specializes in domestic violence, and conducted regular follow-up with the individual. At approximately 30 days after the initial encounter, the Clinician called Luis to check in. Luis had enrolled in outpatient therapy, separated from their partner, and reported doing much better.

The CARE Team responded to an individual in mental health crisis, “Dylan,” who was expressing suicidal thoughts and had locked himself in his living space because he did not want to go to the hospital. The CARE Team engaged Dylan, who was especially receptive to the paramedic on the team. The paramedic was able to take vitals and engage Dylan about his suicidal thoughts. While speaking with the CARE Team, Dylan remained focused on the paramedic, who reassured him that everything he expressed was valid, and that the CARE Team could help him not only in that moment but also by providing follow-up services. Although Dylan remained tearful and somewhat distressed, he gradually began to state that he did not want to die but just wanted something in his life to change. The CARE Team took Dylan to his preferred hospital and followed up 24 hours later to check-in.